Lipedema is a life-altering disease that can greatly impact everyday life for millions of women around the world. Seeking out treatment takes dedication and significant research, and with each treatment option available there are certain risks that must be reviewed. Lymph sparing liposuction is typically a safe and effective procedure when performed by trained hands and all necessary precautions are followed. Current technology allows properly trained vascular, cosmetic plastic surgeons to remove the subcutaneous fat tissue safely and greatly reduce the impact lipedema has on the patient’s mobility as long as specialized surgical techniques are followed which limit injury to an already compromised lymphatic system. However, as with any surgical procedure, there is always a certain amount of risk involved. For patients with a delicate lymphatic system, partnering with a highly skilled and recommended surgeon is even more important.
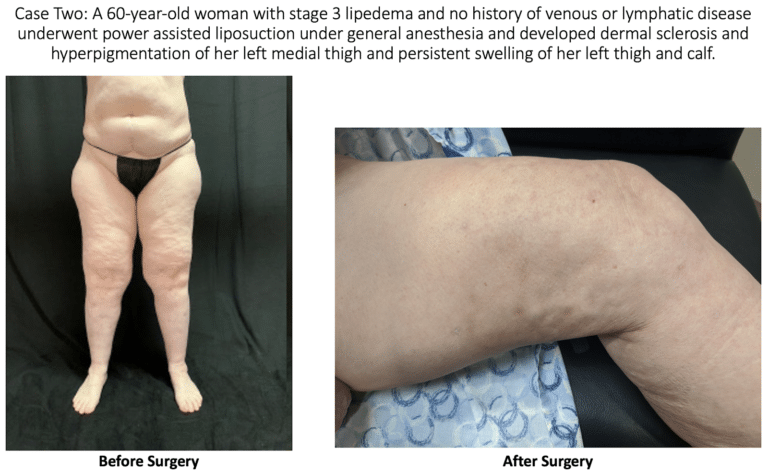
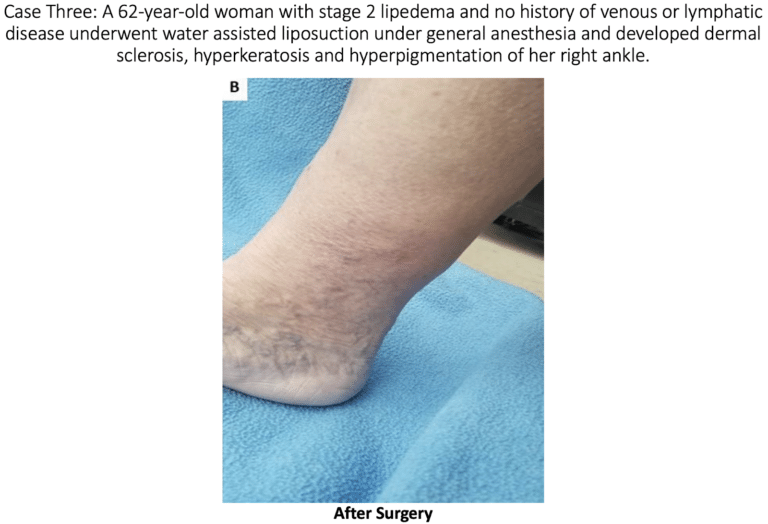
At this year’s annual congress of the American Vein and Lymphatic Society (AVLS), Dr. Wright presented an abstract on lymphatic injury after suction lipectomy in patients with lipedema. The abstract consisted of three cases of patients who had been diagnosed with lipedema and underwent suction lipectomy with ultrasound, power, or water assistance. Immediately after their surgeries, the patients appeared to recover normally; however, over a 3 to 6-month period, they developed skin changes and symptoms consistent with lymphatic injury. Specifically, the patients developed skin lymphostatic fibrosis, papillomatosis, dermal sclerosis and leg swelling.
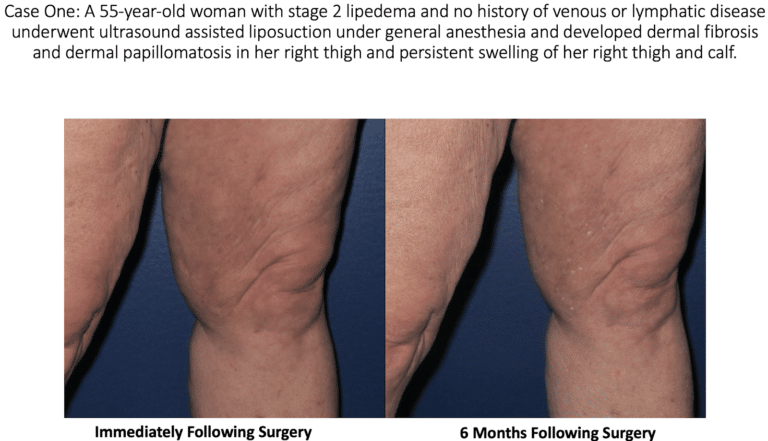
Skin Lymphostatic Fibrosis: This is a widespread side effect in patients with lymphedema, where the skin hardens over time. In the early stages of lymphedema, swelling is soft to the touch. However, over time, the swelling hardens the skin due to the development of connective tissue fibers underneath the skin of the affected areas.
Papillomatosis: The growth of numerous papillomas, more commonly referred to as warts.
Dermal Sclerosis: Hardening and tightening of the skin and connective tissues.
Leg Swelling: Ironically, leg swelling is one of the most common symptoms of lipedema, and what prompts patients to seek treatment. Post lymph-sparing liposuction for lipedema, lymphatic injury can lead back to leg swelling.
At this time, most experts believe that suction lipectomy with ultrasound, power, or water assistance techniques, in the proper hands, are safe and effective treatments for lipedema, as long as the surgeon performing the liposuction has skill and experience to perform a lymph sparing technique. When suction lipectomy is performed properly, it improves symptoms, lymphatic flow and skin health.
Studies have shown that lipedema is often associated with lymphatic impairment. Studies have also shown that lymphatic function is not changed or improved with careful liposuction that uses surgical techniques and technologies that protect or minimize injury to the lymphatics. We do know that traditional liposuction, without special care of the lymphatics or proper tumescent technique, can cause lymphatic damage and possibly worsen lipedema symptoms.
Modified liposuction surgery is the only available technique to correct and remove the abnormal adipose tissue of lipedema. Liposuction is a surgical treatment that involves the application of local (tumescent and water-assisted) anesthesia, and subsequent removal of adipose tissue through a straw-like device called a cannula [4]. One end of the cannula is connected to a vacuum device, and the other end is inserted through a small incision of the skin and removes fat via aspiration.
There are two techniques of liposuction that can be safely used to treat lipedema, provided the surgeon has experience in techniques to avoid injury to the lymphatics. Note: Lipedema patients often have impaired lymphatic function, so great care must be taken to avoid further damage. The two liposuction techniques are safest and most effectively used by surgeons with a great deal of experience with the treatment of lipedema are tumescent liposuction and water-assisted liposuction. These two are the only research-backed surgical treatment plans for lipedema.

- Tumescent liposuction involves the introduction of large volumes of tumescent solution into the fat below the skin space to tumesce (or swell) the area. This solution contains lidocaine anesthetic, which causes local numbness; epinephrine, which causes constriction of blood vessels to reduce the risk of bleeding; and saline, which causes swelling of the adipose tissue and protects the vascular structures from trauma. The solution is allowed to infiltrate the tissue, and its salinity causes the adipose tissue and cells to swell and separate from the connective tissue, at which point the cannula is used to aspirate the fat [1,2,3,4].
- Water-assisted liposuction does not involve over-swelling [tumescence] of the adipose tissue. Instead, small amounts of tumescent solution and water are introduced into the adipose tissue. Once sufficient numbing occurs, a modified cannula with an attached fan-shaped and slightly pressurized saltwater jet is inserted into the subcutaneous space and applied to separate the adipose cells from the tissue, while simultaneously aspirating the solution and detached cells [5].
The skin changes experienced by the above patients were not present prior to the surgery. The changes seen in these patients are consistent with stage 2 or stage 3 lymphedema. We are left to conclude that the lymphedema changes in the skin were most likely the result of surgical trauma during suction lipectomy. Doctors A. Frick, C.C. Campisi and others have shown that there are surgical techniques that can limit the risk of lymphatic injury. [7,8] These case reports show the importance of choosing a surgeon that will take every precaution to not injure lymphatics.
Patients with increased strain on their lymphatics are at an increased risk for lymphatic injury. Liposuction for Lipedema, for example, requires significant care to not injure lymphatics that only a highly trained individual should be trusted with. Patients must be sure to ask their physician what their experience with lymph-sparing liposuction is and what kind of side effects their patients have experienced in the past. These procedures always have associated risks, but they can be reduced when we rely on the most trusted and experienced individuals in the field.
- Rapprich, S., Dingler, A. & Podda, M. Liposuction is an effective treatment for lipedema-results of a study with 25 patients. J. Dtsch. Dermatol. Ges. J. Ger. Soc. Dermatol. JDDG 9, 33–40 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21166777 or Google Scholar Link
- Buck, D. W. & Herbst, K. L. Lipedema: a relatively common disease with extremely common misconceptions. Plast. Reconstr. Surg. Glob. Open 4, e1043 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5055019/ or Google Scholar Link
- Schmeller, W., Hueppe, M. & Meier-Vollrath, I. Tumescent liposuction in lipoedema yields good longterm results. Br. J. Dermatol. 166, 161–168 (2012). Link https://www.ncbi.nlm.nih.gov/pubmed/21824127 and https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2133.2011.10566.x or Google Scholar Link
- Wollina, U., Goldman, A. & Heinig, B. Microcannular tumescent liposuction in advanced lipedema and Dercum’s disease. G. Ital. Dermatol. E Venereol. Organo Uff. Soc. Ital. Dermatol. E Sifilogr. 145, 151–159 (2010). links https://www.ncbi.nlm.nih.gov/pubmed/20467389 and https://www.dovepress.com/treatment-of-elderly-patients-with-advanced-lipedema-a-combination-of–peer-reviewed-fulltext-article-CCID or Google Scholar Link
- Stutz, J. J. & Krahl, D. Water jet-assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic Plast. Surg. 33, 153–162 (2009). Link: https://www.dovepress.com/lipedema-diagnostic-and-management-challenges-peer-reviewed-fulltext-article-IJWH or Google Scholar Link
- Damstra, RJ. First Dutch guidelines on lipedema using the international classification of functioning, disability and health. Phlebology. 2017 Apr;32(3):152-159. or Google Scholar Link Dutch Standard of Care for Lipedema Guidelines: links https://journals.sagepub.com/doi/abs/10.1177/0268355516639421 and https://www.ncbi.nlm.nih.gov/pubmed/27075680
- Frick A, Hoffmann JN, Baumeister RG, Putz R. Liposuction technique and lymphatic lesions in lower legs: anatomic study to reduce risks. Plast Reconstr Surg. 1999 Jun;103(7):1868-73; discussion 1874-5. doi: 10.1097/00006534-199906000-00009. PMID: 10359247.
- Campisi CC, Ryan M, Boccardo F, Campisi C. Fibro-Lipo-Lymph-Aspiration With a Lymph Vessel Sparing Procedure to Treat Advanced Lymphedema After Multiple Lymphatic-Venous Anastomoses: The Complete Treatment Protocol. Ann Plast Surg. 2017 Feb;78(2):184-190. doi: 10.1097/SAP.0000000000000853. PMID: 27404468.