Getting an initial Lipedema diagnosis is a challenge for many women suffering from it. In fact, an overwhelming majority of patients seeking treatment are well into their forties, fifties, sixties, or later in age, simply because they had never heard of lipedema or been diagnosed with it. After decades of being diagnosed with a high Body Mass Index (BMI) followed by a general obesity diagnosis or misdiagnosed as lymphedema, some of these women with lipedema sought alternate explanations for their pain, discomfort, and unsuccessful weight loss, despite regular diet, exercise, and in some advanced cases even after undergoing bariatric surgery.
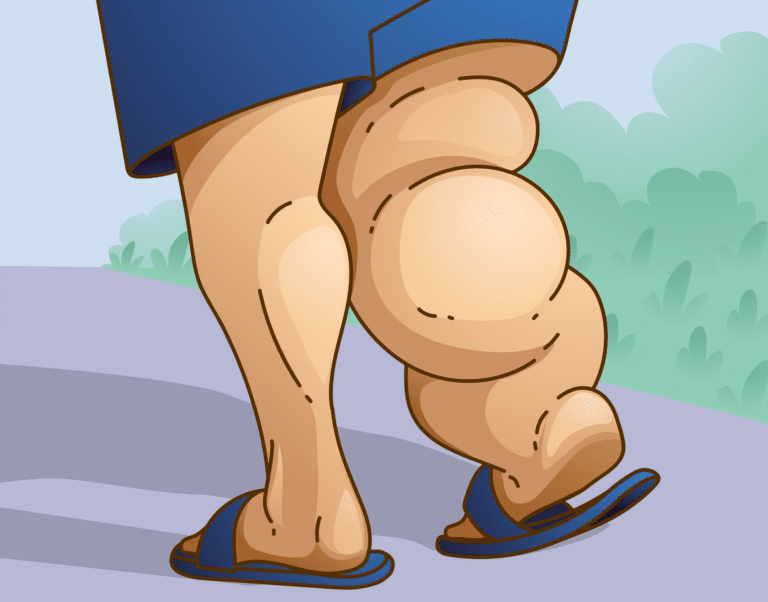
Fat cells, (also referred to as adipose tissue) provide the human body with both cushioning and insulation. Lipedema affects the accumulation of these fat cells in the body, resulting in bulging, irregular fat in the affected areas. The legs are the most commonly affected area, and in many cases, excessive clustering of fat cells is noticed in the arms as well. These fundamental characteristics of lipedema make it increasingly difficult for patients and providers to confuse Lipedema and comorbidities of the disease, especially between Lipedema, Lymphedema, and Phlebolymphedema.
What is Lipedema?
Lipedema is a fat disorder, mainly affecting women, that causes an enlargement of both legs due to deposits of fat under the skin. It’s characterized as a “progressive disorder,” meaning it generally gets worse over time. Sufferers living with lipedema experience easy bruising and tenderness, pain in the affected areas, and significant disability in daily life. In severe and more progressive cases, the trunk and upper body may also be affected, including the arms and upper back. Little is known about the disorder, and it’s often misdiagnosed and incorrectly treated as general obesity.
For anyone affected, diet and exercise alone aren’t effective ways to get rid of Lipedema fat; Lipedema fat has proved relatively immune to these lifestyle changes and won’t budge. While women are likely to experience some weight loss with a healthy diet and regular exercise routines, weight loss is usually mostly loss of non-Lipedema fat. In these instances, the painful, stubborn fat remains. This cycle becomes a difficult one to break for those with the disorder: Yo-yo dieting leads to more weight gain. More weight gain leads to increased pain and disability. Increased pain and disability make it more challenging to manage mobility and secondary obesity increases. Lipedema fat also appears to be relatively resistant to bariatric surgery, meaning many women are undergoing dangerous surgeries without experiencing the intended benefit of significant loss of lipedema fat.
Lipedema vs. Lymphedema
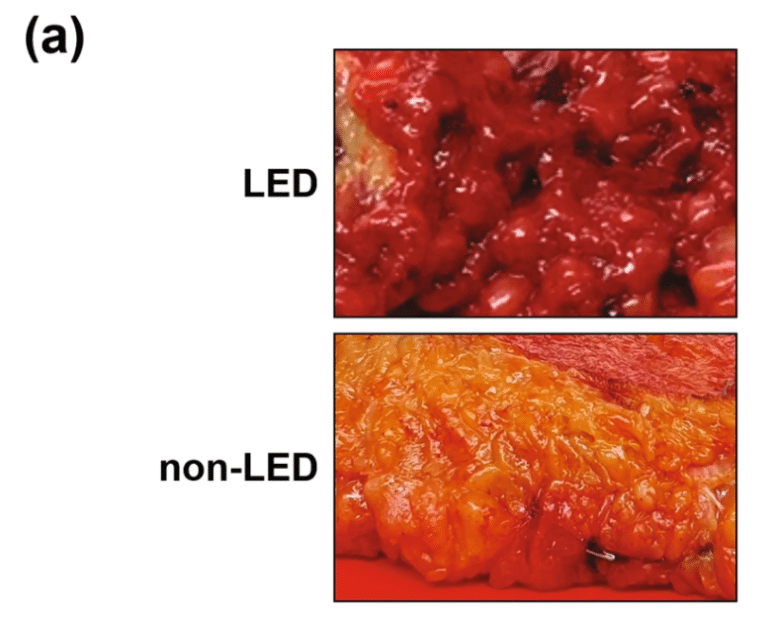
Another misdiagnosis that many women with lipedema experience are lymphedema. Lymphedema is another lymphatic disease that shares similarities with lipedema, but ultimately requires different treatment for successful patient care. Women with lipedema and lymphedema both experience excessive fluid in the affected areas, namely the limbs in both diseases, however, early on lipedema patients tend to have much more fat in the body. Lymphedema presents early on with excessive fluid in the affected area(s) more often in one limb, and as muscles atrophy over time, they begin to turn into fat. Additionally, the tell-tale sign of lymphedema is that the limbs are affected asymmetrically – the slide of the arms cross section below shows the left vs. right arm, with the right affected by lymphedema and experiencing a higher fat level than the left. The second slide of the MRI is that of a patient with lipedema. Not only is the fat content lower, but the legs are affected symmetrically, rather than one greater than the other.
What Is Lymphedema?
Lymphedema in the right leg lymphedema occurs when a clear fluid known as lymphatic fluid builds up and causes fluid retention in the soft tissues of your body. Usually, this occurs in the arms and legs. The lymphatic system consists of lymph vessels and lymph nodes. Lymph vessels collect a fluid that is made up of water, fats, protein, and wastes from the cells of the body. Furthermore, lymph vessels carry this fluid to your lymph nodes. After that, lymph nodes filter waste materials and then recycle the fluid to your blood. However, damaged or missing vessels and nodes cause lymph fluid blockage. In this case, they are unable to cycle through your system. In addition, the fluids can create localized fluid retention and cause swelling, known as lymphedema. This usually affects the arms or legs.
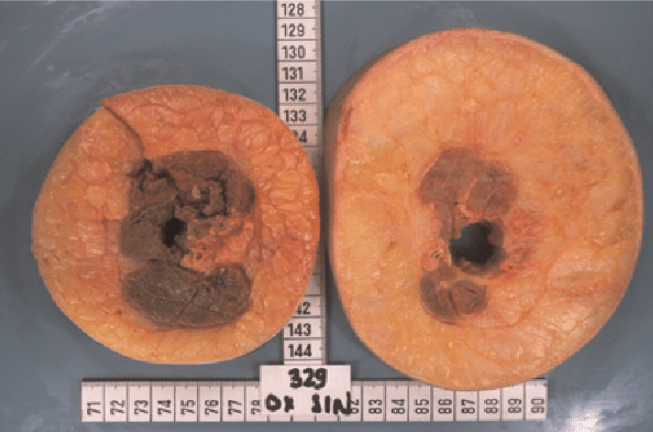
Picture of Crossection of Left [lymphedema] and right arm [normal]. Notice the muscle atrophy and increase subcutaneous fatty tissue on the arm with lymphedema.
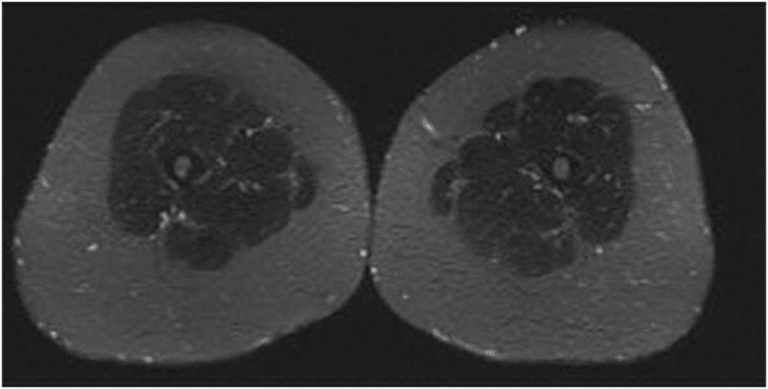
MRI image of two legs with Lipedema. Notice the thickened subcutaneous fatty tissue on both legs. Notice how the lipedema looks much like the above cross-section of lymphedema. Find more from Dr. Wright’s AVLS 2021 Lipedema and BMI Presentation and Reports of Interest.
Furthermore, injuries to your lymphatic system, also known as secondary lymphedema, can cause lymphedema. This is actually the most common form of lymphedema. Unfortunately, people can develop chronic lymphedema, which can last for the rest of their lives. In addition, chronic lymphedema can be difficult to treat with lymphedema therapy and it increases the likelihood hood contracting an infection. Minor injuries to the skin can cause lymphangitis. For example, a cut, scratch, insect bite, or athlete’s foot can create a severe infection if you don’t treat it promptly. Moreover, lymphangitis affects the connective tissue under the skin. Additionally, multiple infections can cause scarring that makes the tissue vulnerable to more swelling and infection. On top of that, advanced chronic lymphedema can lead to fibrosis or hardening of the tissue.
What Are the Symptoms of Lymphedema?
In short, symptoms do not always occur immediately. They can sometimes occur 15 or more years following an injury to your lymphatic system. When symptoms eventually occur, they can include:
- Aching, weakness, redness, heaviness, or tightness in one of your limbs
- Less flexibility in your wrist or ankle
- Tight-fitting rings or shoes
What Causes Lymphedema?
Infection is the most common cause of lymphedema in the legs. The second most common cause is a traumatic injury or surgery. Additionally, other causes of lymphedema to the legs are cancer and hereditary conditions.
What is Phlebolymphedema?
Like Lipedema, Phlebolymphedema is a condition that few have heard of other than recognizing that the word “lymphedema” is part of it. “Phleblo” comes from the word “phlebology”, the study and treatment of venous diseases. Lymphedema, as we know, is a disorder of the lymphatic system that leads to abnormal swelling of the arms, legs, or other parts of the body.

Our veins and the vessels of our lymphatic system may have different jobs in our body, but they’re located very close together. When a patient experiences venous insufficiency that goes untreated, they will eventually experience swelling, skin discoloration, or even painful ulcers in the affected area. When this happens, our lymphatic vessels respond by trying to absorb the excess fluid. As this happens, the vessels are no longer efficiently processing lymph fluid, and it beings to leak out of the soft tissue in the legs, known as lymphedema. When patients experience lymphedema like this as a secondary symptom due to venous insufficiency, it’s known as Phlebolymphedema.
Understanding Treatment for Lipedema, Lymphedema, & Phlebolymphedema
As we’ve discussed, these three diseases can heavily overlap one another in a single patient, and often it’s unclear what the first step for treatment can be. Doctors may not recognize the different diseases at play and offer little to no solutions other than compression therapy. Fortunately, there are treatment options out there, as long as you receive the proper and full diagnosis to determine the best first course of action. Contact Dr. Wright’s team at St. Louis Laser Veins to get started!