Interstitial fluid plays a significant role in the development and progression of lipedema and lymphedema, two chronic swelling conditions that affect millions of people worldwide. In this comprehensive guide, we will explore the nature of the interstitial fluid, its connection to lipedema and lymphedema, and the pathophysiology of these conditions. We will also discuss the importance of early diagnosis, treatment options, and potential complications associated with these disorders.
Interstitial Fluid: A Brief Overview
Interstitial fluid, also known as tissue fluid, is a crucial component of the body’s extracellular fluid. It surrounds and fills the spaces between cells, providing nutrients and oxygen to the cells while also removing waste products. Interstitial fluid plays a vital role in maintaining the body’s homeostasis and overall health.
Interstitial Fluid and Connective Tissue
Connective tissue is integral to the structure of blood and lymphatic vessels, and genetic changes may affect vessel compliance, increasing permeability, especially when under increased pressure. In lipedema, the soft consistency of adipose tissue can be associated with a neurogenic inflammatory state, which further complicates the condition of microangiopathy. The pericellular accumulation of liquid is related to the dilation of the prelymphatic drainage system, which can result in progressive damage to the lymphatic drainage capacity.
Lipedema: A Painful Disease of Excess Loose Connective Tissue
Lipedema is a chronic swelling condition that almost exclusively affects women, causing an overgrowth of fat storage cells (adipocytes) in the limbs. This abnormal fat accumulation typically begins during periods of hormonal flux, such as puberty, pregnancy, or menopause, and worsens by stage, increasing lymphedema risk. Lipedema is characterized by a disproportionate accumulation of fat on the limbs, often causing significant pain and discomfort.
Lipedema Stages
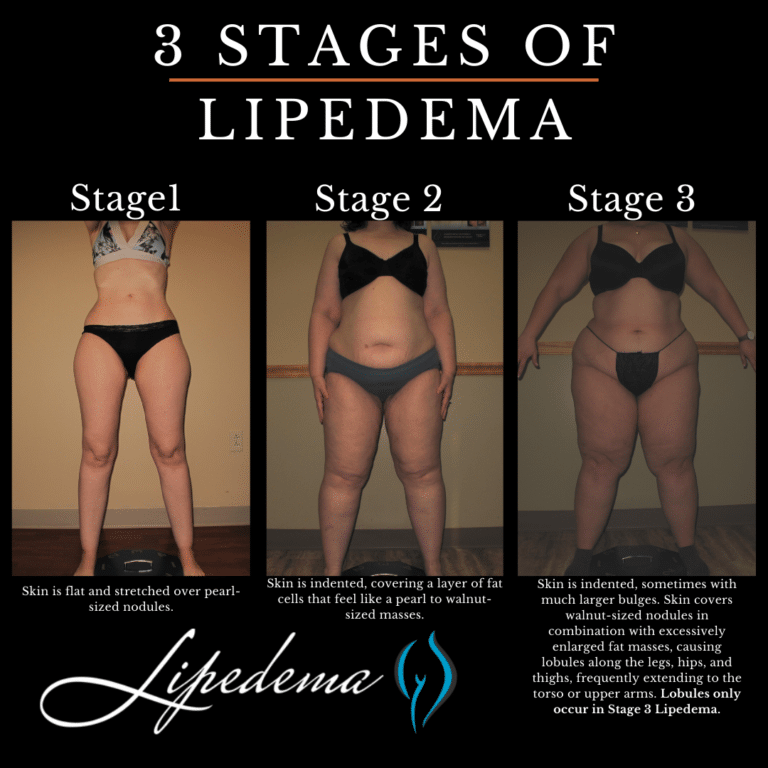
Lipedema progresses through three stages:
- Stage 1: The skin is smooth, but the tissue beneath has a pebble-like feel, indicating fibrosis.
- Stage 2: Similar to Stage 1, but with more lipedema tissue, skin dimpling due to fibrotic changes, and larger nodules.
- Stage 3: Large lobules of lipedema skin and tissue are present, often causing mobility issues.
Lipedema and Interstitial Fluid
Excess interstitial fluid may accumulate in lipedema tissue due to dysfunctional blood vessels (microangiopathy). Increased compliance of connective tissue in higher stages of lipedema may allow fluid to disperse into the interstitial space, including between skin dermal fibers. This excess fluid can contribute to the development and progression of lipedema. Furthermore, many women with lipedema have hypermobile joints, suggesting a connective tissue disorder that may affect vessel structure and tissue compliance, resulting in excess fluid entering the interstitial space.
Lymphedema: A Condition Caused by Ineffective or Absent Lymphatic Fluid Transport
Lymphedema is a chronic swelling condition that results from ineffective or absent lymphatic fluid transport. Interstitial fluid accumulation occurs as a direct result of local or downstream lymphatic insufficiency, leading to the build-up of macromolecular proteins, hyaluronan, lipoproteins, tissue antigens, and cellular metabolites within the extracellular space. The sustained inflammatory response in lymphedema drives fluid deposition towards tissue fibrosis and adipose expansion.
Lymphedema and Interstitial Fluid
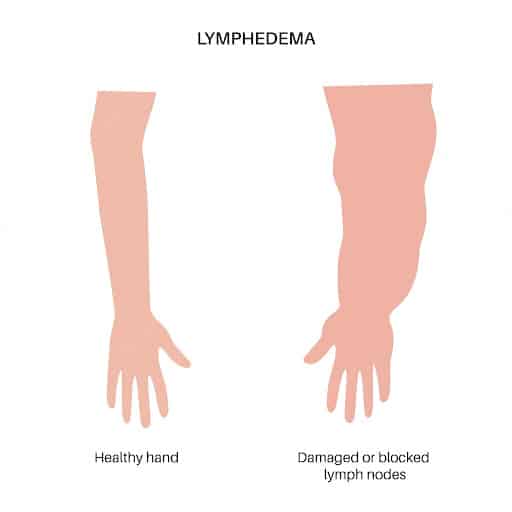
In lymphedema, the interstitial fluid accumulates around vessels and between dermal skin fibers, causing increased pressure and protein concentrations within the affected tissues. This leads to a sustained inflammatory response, characterized by increased expression of cytokines, chemokines, and immune cell accumulation and activation. The resulting tissue remodeling towards fibrosis, along with adipose expansion, further impairs lymphatic function and exacerbates the condition.
The Connection Between Lipedema and Lymphedema
While lipedema and lymphedema are distinct conditions, they share several similarities, including the accumulation of interstitial fluid and the development of tissue fibrosis. In both disorders, interstitial congestion leads to fibrosis, characterized by increased collagen deposition and connective tissue overgrowth. However, the fibrosis patterns differ between the two diseases: diffuse fibrosis in lymphedema and more spaced-out fibers in lipedema, which can lead to secondary lymphedema as the disease progresses.
Diagnosing and Treating Lipedema and Lymphedema
Early diagnosis and appropriate treatment are crucial to managing lipedema and lymphedema and preventing complications. A trained clinician can establish a diagnosis based on physical evaluation and the presence of specific signs and symptoms. Various treatment options are available, including:
- Complete Decongestive Therapy (CDT), involving manual lymphatic drainage, compression garments, therapeutic exercises, and meticulous skin hygiene.
- Weight management to optimize body weight and indirectly reduce the likelihood of disease progression.
- Surgical interventions, such as liposuction or bariatric surgery, in selected cases to reduce the total disease burden and improve mobility and comfort.
Potential Complications and Associations with Other Conditions
Untreated lipedema and lymphedema can lead to various complications, including immobility, infection, joint pain, and psychological distress. Furthermore, lipedema and lymphedema may be associated with other conditions, such as obesity, anorexia nervosa, bulimia, and chronic venous insufficiency. Adequate management of these comorbid conditions is essential for successful treatment and prevention of complications.
Conclusion
Interstitial fluid plays a critical role in the development and progression of lipedema and lymphedema. A better understanding of the mechanisms underlying interstitial fluid accumulation and its impact on these conditions is essential for improving diagnosis, treatment, and management strategies. Early intervention and appropriate treatment can help prevent complications, improve quality of life, and provide relief for those suffering from lipedema and lymphedema.